Will Hcbs Money Be Reinstated After A Spend Down
Home and customs-based services (HCBS) help seniors and people with disabilities and chronic illnesses live independently outside institutions by profitable with daily needs. HCBS include merely are not limited to home health adjutant services, help with self-intendance tasks such as eating or bathing, supportive housing, and assistive technology. People who utilize HCBS include seniors with physical and/or cerebral limitations, people with intellectual disabilities such every bit Down's syndrome or autism, people with concrete disabilities such as spinal string injuries or cognitive palsy, people with serious mental illness, and people with disabling chronic conditions.
The unmet need for HCBS for seniors and people with disabilities pre-dates the COVID-19 pandemic, with Medicaid serving equally the primary source of coverage for HCBS. These services are unaffordable out-of-pocket for many people and unavailable through private insurance or Medicare. The pandemic's disproportionate bear on on seniors and people with disabilities, particularly those living in congregate settings such as nursing homes, has brought heightened focus on the need for boosted HCBS, and the growing elderly population in the coming years will further intensify the demand for these services. Over the last several decades, states have focused on shifting the Medicaid plan's historical bias toward institutional services by devoting an increasing share of their total long-term services and supports (LTSS) spending to HCBS. Spending on HCBS surpassed spending on institutional care for the start time in FY 2013 and comprised 56% of total Medicaid LTSS spending in FY 2018, with substantial variation amidst states.
The American Rescue Plan, the COVID relief parcel recently signed into law by President Biden, includes a provision to increase the federal matching rate (FMAP) for spending on Medicaid HCBS past 10 per centum points from Apr ane, 2021 through March 31, 2022 provided states maintain land spending levels as of Apr 1, 2021. To access the new funds, recent guidance requires states to submit for CMS blessing an initial HCBS spending plan projection and narrative past June 12, 2021, though CMS recently announced that states could request a 30-day extension for their initial submission due date. This brief discusses the new provision and provides state by land estimates of the potential effects of the policy change.
What does the American Rescue Program do for HCBS?
The HCBS provision in the American Rescue Plan increases the federal matching rate (FMAP) for Medicaid HCBS spending past 10 per centum points from Apr 1, 2021 through March 31, 2022. The police specifies that states must use the enhanced funds to "implement, or supplement the implementation of, i or more activities to enhance, expand, or strengthen" Medicaid HCBS. CMS guidance released on May 13, 2021 confirms that the enhanced funds must be used for activities "across what is available under the [state's] Medicaid program as of April 1, 2021." While the final version of the law did non detail specific activities, the CMS guidance provides a not-exhaustive listing of initiatives that states might fund, including activities to come across HCBS needs created by COVID-nineteen and activities to build land HCBS chapters and advance LTSS rebalancing reforms. For example, in response to COVID-19, states might use the enhanced funds to aggrandize covered services to reduce the run a risk of institutionalization, facilitate COVID-19 vaccine access for HCBS enrollees, or back up the directly care workforce. To build HCBS chapters and accelerate LTSS rebalancing, states might streamline eligibility and enrollment processes, increase covered services, aggrandize the direct care workforce, or serve boosted HCBS enrollees. (Figure 1). States have until March 31, 2024 to spend the enhanced funds. The Appendix Table contains a detailed summary of the activities included in the CMS guidance.
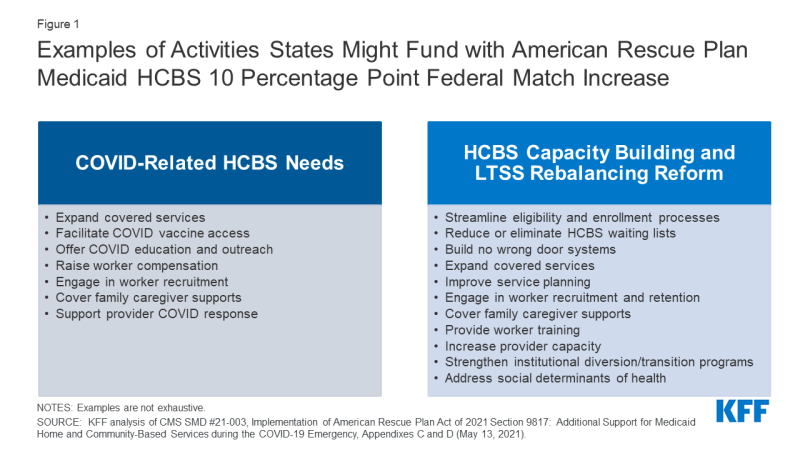
Figure one: Examples of Activities States Might Fund with American Rescue Program Medicaid HCBS ten Percentage Point Federal Match Increase
The law increases the full dollars available for Medicaid HCBS, equally states are required to maintain their current HCBS spending to qualify for the enhanced federal funds. Specifically, states must maintain their level of HCBS spending equally of April 1, 2021. CMS guidance confirms that states "cannot use land funds equivalent to the corporeality of federal funds made available by the increased FMAP to pay for HCBS that [are] available nether the[ir] Medicaid program equally of April 1, 2021." The Appendix provides more particular almost the conditions states must run into to satisfy this requirement according to CMS guidance. The proposed x percent point increment for HCBS will exist added to the land's regular Medicaid matching rate (which ranges from 50% to 78% in FY 2022), besides as to other FMAP increases bachelor to states, including the six percentage point increase for Community First Selection attendant intendance services, the 6.2 percentage indicate increase provided to address the COVID-19 public wellness emergency (PHE) nether the Families Kickoff Coronavirus Response Act, any disaster recovery FMAP (available to states with a federally alleged disaster and a certain amount of FMAP decline), and the ninety% federal matching rate for Medicaid expansion adults nether the ACA, as well as the new five percentage indicate increment in the regular matching rate for states newly adopting the ACA expansion provided in a carve up section of the law. The cumulative enhanced matching rate for Medicaid HCBS under the law is capped at 95%.
What is the estimated effect of the American Rescue Plan HCBS funding for states?
Nosotros estimate that nationally, federal spending for HCBS could increase by near $xi.4 billion (Table 1). This estimate is similar to that put out past the Congressional Budget Office, which estimated increased federal costs of approximately $12.7 billion. In the time period that the FMAP increase would be in effect (the terminal two quarters of FY 2021 and the first two quarters of FY 2022), we gauge that total federal and country Medicaid HCBS spending will be approximately $114 billion (Table 1). Estimated total Medicaid HCBS spending varies widely by state, ranging from $198 million dollars in Wyoming to nearly $22 billion in California. The boosted $11.4 billion federal dollars from this FMAP increment would be distributed proportional to the size of land HCBS programs, with California receiving nearly $ii.2 billion additional federal dollars and Wyoming receiving near $19.eight meg additional federal dollars. This wide land variation reflects both state size and various land policy choices on HCBS programs, well-nigh all of which are offered at land option.
These estimates are fabricated with a degree of uncertainly. Our estimates reflect HCBS spending in FY 2021 and FY 2022 based on inflation rates from CBO'due south projected spending on Medicaid LTSS. All the same, these estimates practice non account for states expanding underlying HCBS spending beyond current levels due to the additional federal incentive. Additionally, some spending in some states may not be eligible for the full increase, should the state hitting the 95% federal friction match cap, after accounting for the 10 percentage point increase in the nib every bit well as other enhanced matching rates available to states, such as the enhanced match for the ACA Medicaid expansion group. These estimates presume that all states maintain their current spending levels, as required by the law.
| Methods |
| This data note uses spending data from KFF'south FY 2018 HCBS program surveys and FY 2018 Medicaid expenditure data from CMS Financial Direction Reports to estimate the amount of additional federal funds available to each country under the proposed FMAP increment. The estimates rely primarily on land-reported information from KFF'due south FY 2018 HCBS program survey for expenditures on home wellness, personal care, Community Get-go Choice, and Department 1915 (i) state plan services as well as HCBS expenditures provided through Section 1915 (c) and Section 1115 waivers. These categories make upward the vast bulk of Medicaid HCBS spending, and our estimates include capitated spending in these categories. There are as well several additional HCBS categories identified in the police that are eligible for the HCBS match just are not covered by our almanac HCBS survey. These categories are Footstep, Section 1915 (b) primary intendance instance management, Section 1915 (j) personal care aid, state plan case direction services, and state plan rehabilitative services. FY 2018 spending for these additional categories are pulled from FY 2018 CMS-64 reports and reflect only fee-for-service spending. These totals reflect about $vii.5 billion out of a total of $100 billion in estimated Medicaid HCBS spending in FY 2018. HCBS spending was then summed across all program government to place Medicaid HCBS country totals for FY 2018. The estimates practice not include state spending for individual duty nursing services provided in a casher'due south home, which are eligible for the HCBS match according to CMS'south May 2021 guidance. These totals were inflated using CBO's projected Medicaid LTC spending baseline from FY 2019 to FY 2022. Since CBO'due south current published estimates do not include baseline Medicaid LTC spending for FY 2018, the same amount of growth was used to estimate spending from FY 2018 to FY 2019 as FY 2019 to FY 2020. Almanac growth rates using CBO's Medicaid LTC baseline range from 3.0% to 4.ii% from FY 2019 – FY 2022. Total Medicaid HCBS spending for the four quarters during which this additional federal match would be available reflects one-half of estimated Medicaid HCBS spending from FY 2021 and half of the estimated Medicaid HCBS spending from FY 2022, which amounts to approximately $114 billion (Table one). Boosted federal dollars available through the proposed FMAP bump are calculated by taking 10% of estimated state and national totals from this time menses. Nosotros assume that this law is intended to provide fiscal relief with a stipulation that states employ new funds from the FMAP increase to "supplement and not supervene upon" current land spending. The estimates do not reverberate the opportunity outlined in CMS's May 2021 guidance for states to receive boosted enhanced federal funding. According to the guidance, states receive the 10 per centum indicate enhanced federal matching funds when they submit claims for HCBS from April 1, 2021 through March 31, 2022. Once states receive the enhanced federal matching funds, that money is considered to be state funds. In the guidance, CMS explains that states can and so use those state funds (equivalent to the amount of enhanced federal funds they have drawn down) to provide additional Medicaid-covered HCBS (beyond what was covered equally of Apr 1, 2021). If states utilize funds in this way, they can receive the increased FMAP on that spending one additional time for claims paid betwixt Apr one, 2021 and March 31, 2022. |
| Table 1: Estimated Boosted Federal Dollars for Medicaid HCBS Nether American Rescue Act HCBS FMAP Bump | ||
| State | Estimated Medicaid HCBS Spending – April 1st, 2021 – March 31st, 2022 | Estimated Additional Federal Dollars for Medicaid HCBS |
| Usa TOTAL | $113,828,064,000 | $11,382,811,000 |
| Alabama | $871,267,000 | $87,127,000 |
| Alaska | $374,649,000 | $37,465,000 |
| Arizona | $1,797,659,000 | $179,766,000 |
| Arkansas | $1,178,098,000 | $117,810,000 |
| California | $21,694,742,000 | $2,169,474,000 |
| Colorado | $1,539,931,000 | $153,993,000 |
| Connecticut | $i,944,728,000 | $194,473,000 |
| DC | $892,504,000 | $89,250,000 |
| Delaware | $372,613,000 | $37,261,000 |
| Florida | $3,195,868,000 | $319,587,000 |
| Georgia | $1,555,865,000 | $155,587,000 |
| Hawaii | $275,132,000 | $27,513,000 |
| Idaho | $534,865,000 | $53,487,000 |
| Illinois | $1,770,892,000 | $177,089,000 |
| Indiana | $1,395,860,000 | $139,586,000 |
| Iowa | $931,020,000 | $93,102,000 |
| Kansas | $one,400,775,000 | $140,078,000 |
| Kentucky | $968,416,000 | $96,842,000 |
| Louisiana | $906,192,000 | $xc,619,000 |
| Maine | $601,967,000 | $lx,196,000 |
| Maryland | $2,344,175,000 | $234,418,000 |
| Massachusetts | $4,092,432,000 | $409,243,000 |
| Michigan | $ane,391,405,000 | $139,141,000 |
| Minnesota | $four,886,088,000 | $488,609,000 |
| Mississippi | $538,547,000 | $53,855,000 |
| Missouri | $2,286,356,000 | $228,636,000 |
| Montana | $323,827,000 | $32,383,000 |
| Nebraska | $484,708,000 | $48,471,000 |
| Nevada | $605,863,000 | $60,586,000 |
| New Hampshire | $433,200,000 | $43,320,000 |
| New Jersey | $ane,726,932,000 | $172,693,000 |
| New United mexican states | $836,622,000 | $83,662,000 |
| New York | $12,609,573,000 | $1,260,957,000 |
| N Carolina | $one,823,280,000 | $182,328,000 |
| North Dakota | $316,001,000 | $31,600,000 |
| Ohio | $iv,344,503,000 | $434,450,000 |
| Oklahoma | $660,643,000 | $66,064,000 |
| Oregon | $ane,240,435,000 | $124,044,000 |
| Pennsylvania | $seven,291,355,000 | $729,136,000 |
| Rhode Island | $338,718,000 | $33,872,000 |
| South Carolina | $847,649,000 | $84,765,000 |
| South Dakota | $202,815,000 | $twenty,282,000 |
| Tennessee | $one,569,796,000 | $156,980,000 |
| Texas | $eight,621,124,000 | $862,112,000 |
| Utah | $468,343,000 | $46,834,000 |
| Vermont | $482,800,000 | $48,280,000 |
| Virginia | $2,133,627,000 | $213,363,000 |
| Washington | $2,530,236,000 | $253,024,000 |
| Westward Virginia | $626,949,000 | $62,695,000 |
| Wisconsin | $3,369,435,000 | $336,944,000 |
| Wyoming | $197,584,000 | $19,758,000 |
| NOTES: Estimates are based on estimates of Medicaid HCBS spending in FY 2021 and FY 2022. Run into Methods for more details. SOURCES: KFF estimates based on KFF FY 2018 Medicaid HCBS Plan Surveys, FY 2018 Expenditure Reports From MBES/CBES, and FY 2019 – FY 2022 CBO Medicaid Baseline Projections | ||
Source: https://www.kff.org/medicaid/issue-brief/potential-impact-of-additional-federal-funds-for-medicaid-hcbs-for-seniors-and-people-with-disabilities/
Posted by: culpepperconifice88.blogspot.com

0 Response to "Will Hcbs Money Be Reinstated After A Spend Down"
Post a Comment